Health care access refers to the ability of individuals to obtain necessary medical services and resources. It encompasses various dimensions, including the availability of health services, affordability, geographic location, and the influence of social determinants of health. The significance of health care access lies in its direct correlation with health outcomes; disparities in access can lead to inequitable health results among different populations. To comprehend the complexities of health care access, it is essential to examine each dimension and its implications.
The availability of health care services is a foundational aspect of access. This means that individuals must have health care providers, hospitals, and clinics within reachable distances, offering a range of necessary services. Areas with limited health facilities often experience poorer health outcomes as residents may face challenges in receiving timely and appropriate care. Additionally, the types of services available can vary significantly between urban and rural settings, impacting overall community health.
Affordability also plays a critical role in health care access. Even when health services are available, financial constraints can prevent individuals from seeking necessary care. High out-of-pocket costs, lack of insurance, or inadequate coverage can act as barriers, especially for low-income families. Addressing affordability through policy interventions is essential to ensure that all individuals can access health care services without facing financial hardship.
Geographic And Economic Factors
Geographic and economic factors add another layer of complexity, as individuals residing in rural or underserved areas may experience significant challenges in accessing quality health services. Transportation barriers, limited provider networks, and longer distances to care can further exacerbate these inequities. Lastly, social determinants of health, including education, employment, and living conditions, significantly influence health care access. These factors contribute to systemic disparities, impacting individual and community health outcomes. Understanding these dimensions is crucial for creating targeted solutions that promote health equity and enhance access to health care for all individuals.
Health Care Access in Developed Countries
In developed nations, health care is typically more accessible due to established systems and reliable funding. Countries like the United States and those in Western Europe provide extensive health services, primarily funded through taxes or insurance models. However, disparities often exist, particularly for lower-income populations and marginalized communities. Access may be hindered by high costs, lack of insurance, or geographic barriers.
Health Care Access in Developing Countries
Conversely, in many developing countries, health care access presents a more complex challenge. Limited resources, inadequate facilities, and a shortage of qualified health personnel contribute to significant obstacles. For many, achieving access to necessary health services is a struggle. International organizations and local governments work to improve access through initiatives aimed at building infrastructure and offering training.
While progress for Health Care Systems by Country is being made globally, achieving equitable health care access remains a pressing challenge. Continued collaboration among nations and focused investments in health care infrastructure, technology, and workforce development are essential to bridge the accessibility gap and ensure that everyone, regardless of location or circumstance, can receive the care they need. Closing this gap will also require innovative policy reforms that address long-standing systemic barriers to care. Only by integrating local insights with global efforts can we craft sustainable health systems that prioritize inclusivity and long-term well-being.
Impact of Limited Health Care Access
Limited health care access presents significant consequences for individuals and communities, manifesting in adverse health outcomes, economic repercussions, and broader public health implications. Addressing these inequities is vital to improving health outcomes and enhancing economic stability and resilience. Urgent systemic changes in health care access are essential to rectifying these disparities.
- One primary effect is the increase in morbidity and mortality rates among populations lacking adequate access to health services. Individuals with limited health care access often experience delayed diagnoses and treatment, resulting in diseases advancing to more severe stages that are subsequently harder to treat and manage.
- Furthermore, the rise of chronic diseases such as diabetes, hypertension, and heart disease is a crucial factor tied to inadequate health care access. Individuals without regular access to preventive care may not receive the necessary screenings or management strategies to control these conditions effectively. This delay not only exacerbates the health challenges faced by these individuals but also leads to a domino effect in community health, contributing to the overall strain on local health care systems.
- The mental health implications of restricted health care access cannot be overlooked. With insufficient resources for mental health services, individuals may face heightened levels of anxiety, depression, and other mental health disorders, leading to diminished quality of life. This lack of mental health awareness and support can perpetuate a cycle of health inequity, particularly in marginalized communities that already face socioeconomic challenges.
- Moreover, the economic implications of limited health care access are substantial. The burden on public health systems rises due to untreated conditions requiring costly emergency care. Additionally, workplace productivity declines as individuals struggle with persistent health issues. Employers face increased absenteeism and reduced efficiency, contributing to broader economic downturns.
Factors Contributing to Health Care Inequities
Health care inequities stem from a multitude of interconnected factors that significantly affect individuals’ access to essential services. Such systemic issues reinforce a cycle of inequity that continues to impact access to health care for several vulnerable groups, necessitating comprehensive strategies for resolution.
- One of the primary determinants is socio-economic status, which encompasses income level, education, and employment. Those with lower socio-economic status often face significant barriers to accessing quality health care. For instance, individuals in lower income brackets may lack health insurance coverage, which restricts their ability to afford necessary medical care, medications, and preventive services. This financial strain not only limits access but also contributes to poorer health outcomes in this demographic.
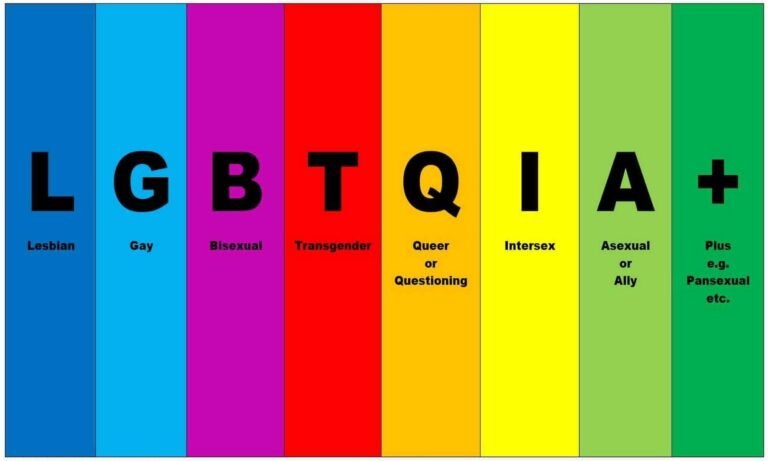
- Race and ethnicity further complicate the landscape of health care access. Numerous studies have shown that racial and ethnic minorities frequently encounter systemic disadvantages in health care delivery. These can manifest in various ways, including discriminatory practices by healthcare providers, language barriers, and a lack of culturally competent care. Consequently, these factors exacerbate existing health disparities, leading to diminished trust in the health care system among marginalized groups.
- Geographical location plays a pivotal role as well, especially in rural and underserved urban areas where health care resources may be scarce. Individuals residing in these regions may have limited access to health facilities, specialists, and even basic services. The distance to the nearest hospital or clinic can deter individuals from seeking timely care, ultimately affecting their overall health.
- Additionally, systemic barriers within the health care system perpetuate these inequities. Structural factors such as inadequate funding, inequitable distribution of healthcare resources, and policies that do not account for the diverse needs of populations contribute to ongoing disparities.
Strategies to Improve Health Care Access Equity
Improving health care access equity requires a multifaceted approach involving policy changes, community engagement, and technology integration. A collaborative effort among government, health care providers, and community organizations is essential in creating equitable systems. By harnessing each sector’s strengths, stakeholders can develop strategies that improve health care delivery and uplift underserved populations. This proactive, strategic approach fosters hope for overcoming challenges and achieving optimal health care access for all.
- First and foremost, policy recommendations play a pivotal role in addressing systemic barriers. Governments should evaluate existing health care policies to identify gaps that disproportionately affect underserved populations. Implementing policies that expand Medicaid and subsidize health insurance for low-income individuals can significantly enhance access. Additionally, advocating for the allocation of resources to rural and marginalized urban areas ensures that health facilities are well-equipped and accessible.
- Community-based interventions are equally vital in bridging health care access gaps. Local organizations can work collaboratively with health care providers to develop outreach programs tailored to the specific needs of the community. Initiatives such as mobile clinics, health fairs, and educational workshops can foster awareness about available services and encourage preventive care. Moreover, culturally competent care practices, which take into account the unique backgrounds and preferences of diverse populations, can help build trust and improve patient engagement within communities.
- The role of technology must also be highlighted when discussing health care access equity. Innovative solutions, such as telemedicine, allow for the delivery of services to patients who may face transportation or mobility issues. By providing virtual consultations, patients can receive care without the need to navigate challenging access routes. Additionally, digital platforms can be used to disseminate health information widely, ensuring that individuals are informed about their health options. The implementation of electronic health records (EHR) systems can facilitate communication and continuity of care among providers, further enhancing access.
What’s More
The posts in My Blog feature reflective, story-driven pieces rooted in personal and societal insights.
The topics in My Interests explore abstract, philosophical ideas and their cultural and societal impact.
👁️ 8,997 Views